Hear the Silent Sufferers: Palliative Care and Pain Relief as Human Rights
By Tamar Ezer & Kiera Hepford

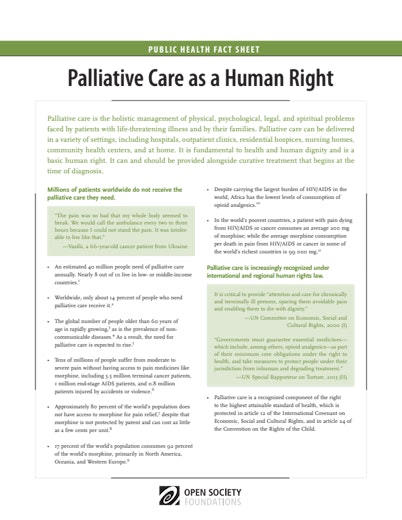
As we observe Human Rights Day, we should not forget the silent sufferers—the millions of people with life limiting illness like AIDS or cancer, who quietly live and die in excruciating, untreated pain.
According to the World Health Organization (WHO), 80 percent of the world population has insufficient access to treatment for moderate to severe pain—or none at all. And, access to pain relief is not equal. Low and middle income countries account for only 6 percent of morphine use worldwide, and yet half of all cancer patients and 95 percent of all new HIV infections are in these countries. 32 out of 57 African countries have almost no morphine availability at all. All of this is despite WHO’s designation of morphine as an essential medicine, as well as increased recognition that pain management and palliative care are fundamental human rights.
These aren’t just statistics—these are stories of individual lives. In the video above, Vlad from Ukraine suffered unrelenting pain from incurable brain cancer because of bureaucratic restrictions.
Another Ukrainian cancer patient, Vasili, reported, “The pain was so bad that my whole body seemed to break. We would call the ambulance every 2 to 3 hours because I could not stand the pain. It was intolerable to live like that.” In India, a patient suffering from vascular disease found the pain so severe that he attempted to hang himself, failing only because his young children heard the noise in time to save him.
Much of this suffering is unnecessary. Severe pain can be effectively and safely managed with oral morphine, which is not protected by patent and can be produced for as little as $.01 per milligram. And palliative care can be provided in all care settings. It is highly effective at treating physical symptoms like pain, and provides psychological, social, and legal support for patients and families, helping them cope with anxieties, as well as spiritual and legal questions. In the eloquent words of one of its founders, palliative care focuses on “adding life to the days rather than days to the life.”
Nonetheless, government health policies frequently neglect the palliative care needs of patients with chronic and incurable illness. Many countries request inadequate supplies of medication from the International Narcotics Control Board. For example, Burkina Faso requested only enough morphine in 2009 to treat eight cancer or HIV patients—but the need exceeded 25,000 people. Even worse, governments actively impede access to pain relief through a slew of restrictive regulations enacted in the name of cracking down on illicit drug use. In Mexico, doctors must obtain special bar coded stickers to prescribe opioid medications, which can only be obtained in state capitals and in limited quantities. In Georgia, these medicines are only stocked at the police station. And in many countries, basic training in pain management and palliative care is unavailable.
In failing to address palliative care needs, many countries are failing to honor human rights. As the UN Special Rapporteurs on the Highest Attainable Standard of Health and on Torture, Cruel, Inhuman and Degrading Treatment have said: “The failure to ensure access to controlled medicines for the relief of pain and suffering threatens fundamental rights to health and to protection against cruel, inhuman and degrading treatment.” The UN Committee on Economic, Social and Cultural Rights has affirmed the importance of “attention and care for chronically and terminally ill persons, sparing them avoidable pain and enabling them to die with dignity.” This concept of dignity is fundamentally at the heart both palliative care and human rights. And in the June 2011 Human Rights Council side meeting on “Access to Palliative Care: A Neglected Component of the Right to Health,” palliative care experts from India, Africa, and Latin America clarified that access to palliative care medicines is a core component of the right to health.
Access to palliative care is a fundamental human rights question. The barrier to palliative care is not a question of resources or technology. There are effective and cheap medicines to treat pain. Rather, it’s a question of political will. Moreover, as Diederik Lohman, Senior Researcher at Human Rights Watch explains, “Looking at palliative care from a rights perspective is about giving voice to people who are dying in their homes and villages from cancer, who do not have the ability to go out into the streets crying out, ‘We are in pain. Government, what are you doing to make sure that I don’t have to suffer?’ These people are mostly invisible, and one of the reasons that palliative care has been neglected over the years is that a cancer patient who is dying simply doesn’t have a voice.”
This Human Rights Day, UN Secretary-General Ban Ki-moon declared, “International law is clear: No matter who you are, or where you live, your voice counts.” We hope you will help us give voice to the silent sufferers by joining palliative care advocates from around the world in this struggle. Visit the Stop Torture in Health Care website to learn more about this issue and the work being done to address the problem on global, regional, and national levels.
Until June 2016, Tamar Ezer was deputy director of the Law and Health Initiative of the Open Society Public Health Program.
Until September 2014, Kiera Hepford was a program officer with the Open Society Public Health Program.